What is Chronic Kidney Disease (CKD)?
Chronic Kidney Disease (CKD) is a long-term condition where the kidneys are damaged and gradually lose their ability to function properly over a period of months or years.
The primary job of your kidneys is to filter waste products and excess fluid from your blood, which are then removed from your body as urine. When kidney function is impaired, this waste can build up to high levels in your blood, which can make you feel sick and cause other serious health problems.
Main Causes of CKD
The two most common causes of chronic kidney disease are:
- Diabetes: High blood sugar levels over time can damage the tiny filters in the kidneys.
- High Blood Pressure (Hypertension): Over time, high blood pressure can damage the blood vessels in and leading to your kidneys, reducing their ability to work properly.
Other conditions that can cause CKD include:
- Autoimmune diseases, such as lupus
- Polycystic kidney disease, an inherited condition
- Glomerulonephritis, an inflammation of the kidney’s filters
- Recurrent kidney infections
- Prolonged obstruction of the urinary tract (from kidney stones or an enlarged prostate)
- Long-term use of certain medications, such as some pain relievers (NSAIDs)
Symptoms of CKD
CKD is often called a “silent” disease because most people have no symptoms in the early stages. Symptoms usually don’t appear until the kidneys are significantly damaged.
In the more advanced stages, symptoms can include:
- Fatigue, weakness, and feeling tired
- Swelling in the feet, ankles, or hands (called edema)
- Shortness of breath
- Persistent itching or dry skin
- Nausea and vomiting
- Loss of appetite
- Muscle cramps, especially at night
- Changes in urination (peeing more or less often, or foamy urine)
The 5 Stages of CKD
Doctors measure kidney function using a blood test that calculates the estimated Glomerular Filtration Rate (eGFR). This number is used to determine the stage of kidney disease:
- Stage 1: Mild kidney damage, but the kidneys are still working well (eGFR 90 or higher).
- Stage 2: Mild kidney damage with a slight loss of function (eGFR 60-89).
- Stage 3a & 3b: Moderate kidney damage and loss of function (eGFR 30-59). This is often when complications like high blood pressure and anemia can start to appear.
- Stage 4: Severe kidney damage and poor function (eGFR 15-29).
- Stage 5: Kidney failure (eGFR less than 15). This is also called End-Stage Renal Disease (ESRD).
Common Herbs useful in CKD
| Herb (Sanskrit Name) | Botanical Name | Traditional Benefits in CKD |
| Punarnava | Boerhaavia diffusa | Known as a potent diuretic (Mutrala) and rejuvenator (Rasayana). It helps reduce swelling (edema) and fluid retention, supports the flushing out of excess toxins, and has anti-inflammatory properties. |
| Gokshura | Tribulus terrestris | Supports genitourinary health, helps detoxify the urinary system, reduces inflammation, and is traditionally used to manage urinary flow issues and kidney stones. It is considered a Rasayana for the urinary tract. |
| Varuna | Crataeva nurvala | Used traditionally for urinary disorders and its lithotriptic (stone-dissolving) properties. It helps reduce kidney inflammation and promotes a healthy urine flow. |
| Guduchi (Giloy) | Tinospora cordifolia | A powerful rejuvenator (Rasayana) and immunomodulator. Its antioxidant and anti-inflammatory properties help protect the kidneys from damage caused by toxins and support overall vitality. |
| Kaasni | Cichorium intybus | Valued for its nephroprotective and cooling properties. It supports kidney filtration and is also beneficial for liver function, which is often related to kidney health. |
Other Supportive Herbs
- Haridra (Turmeric): Known for its active compound, Curcumin, which has remarkable anti-inflammatory and antioxidant properties to help manage renal inflammatory diseases.
- Triphala: A combination of three fruits (Amalaki, Haritaki, Bibhitaki), used as a gentle detoxifier that strengthens the liver and kidneys.
- Shilajit: A mineral-rich resin with rejuvenative and adaptogenic properties that may help improve overall kidney function and enhance immunity.

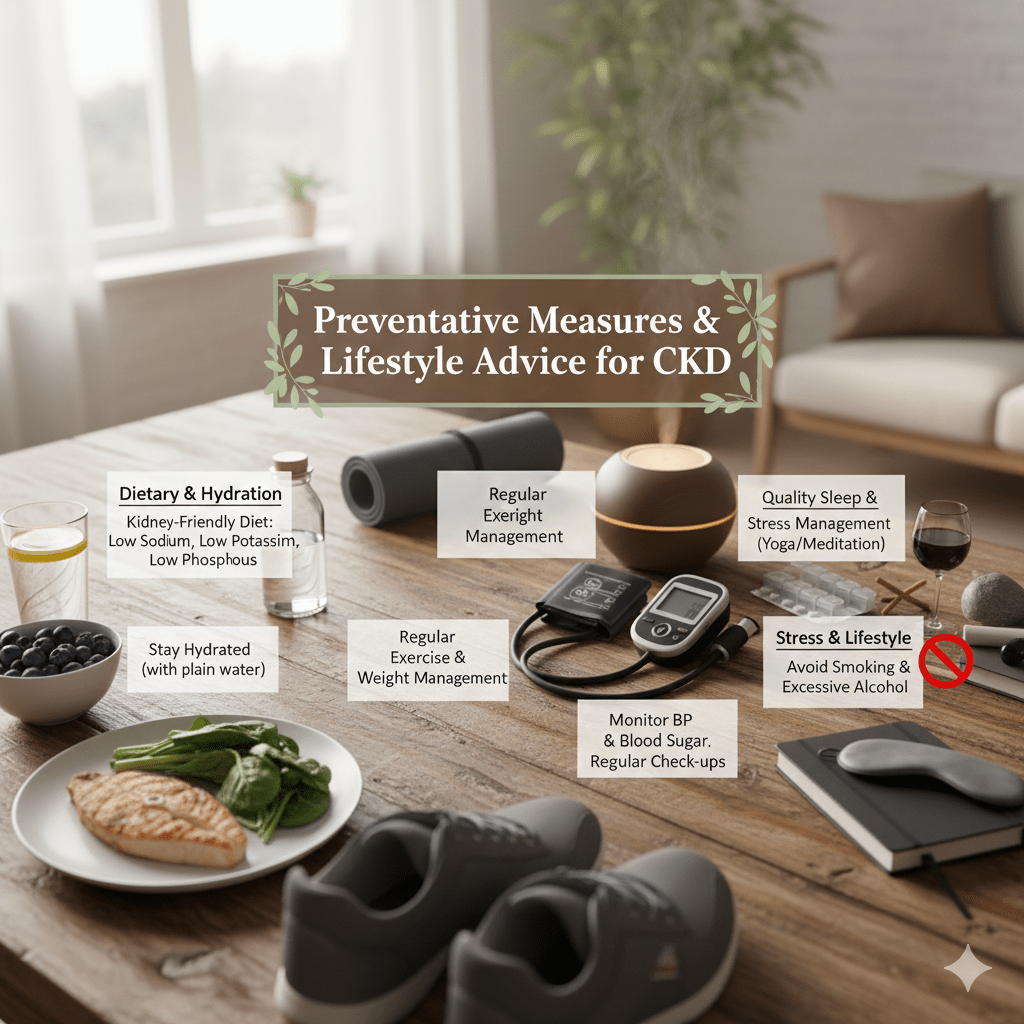
Preventive Measures and Lifestyle Advice
1. Dietary Adjustments
What you eat has a direct impact on your kidney workload.
- Limit Sodium (Salt): High salt intake increases blood pressure and causes fluid retention.
- Goal: Aim for less than 2,300 mg of sodium per day (about 1 teaspoon of salt).
- Tip: Avoid processed foods (canned soups, frozen meals, deli meats) and flavor food with herbs, spices, lemon juice, or vinegar instead of salt.
- Manage Protein Intake: Eating too much protein can make kidneys work harder to filter waste.
- Recommendation: Moderate your protein consumption. Shift towards smaller portions of high-quality protein (eggs, fish, poultry) and incorporate more plant-based proteins (beans, nuts, lentils), which create fewer waste products.
- Monitor Potassium and Phosphorus:Note: This usually applies to later stages of CKD; consult your doctor before restricting these.
- Potassium: If levels are high, limit foods like bananas, potatoes, oranges, and tomatoes. Choose apples, berries, and cabbage instead.
- Phosphorus: Excess phosphorus can weaken bones. Limit dairy, dark colas, and processed foods with phosphate additives.
- Stay Hydrated (Wisely):
- For most people, drinking water is vital to flush out toxins. However, in advanced CKD or heart failure, you may need to restrict fluid intake to prevent swelling. Follow your nephrologist’s specific advice on daily fluid limits.
2. Lifestyle Modifications
Daily habits play a major role in slowing kidney damage.
- Control Blood Pressure: High blood pressure is the #2 cause of kidney failure.
- Target: Generally, aim for below 130/80 mmHg (check with your doctor for your specific target).
- Manage Blood Sugar (Diabetes): Diabetes is the #1 cause of kidney failure. High blood sugar damages the filtering units in the kidneys.
- Action: Monitor your hemoglobin A1C regularly and keep blood sugar within your target range.
- Quit Smoking: Smoking slows blood flow to the kidneys and interferes with blood pressure medications. Quitting is one of the most effective ways to protect kidney function.
- Exercise Regularly:
- Aim for 30 minutes of moderate activity (walking, swimming, cycling) at least 5 days a week. Exercise helps control blood pressure and blood sugar.
- Maintain a Healthy Weight: Obesity forces kidneys to work harder to meet the body’s metabolic demands. Losing even a small amount of weight can reduce this strain.